A Guide to Getting Serious About Bio-Lab Safety
Over the past several weeks, U.S. President Donald Trump and Secretary of State Mike Pompeo have repeatedly suggested that the virus that causes COVID-19 may have leaked from a biological laboratory in China rather than naturally spreading from animal to human hosts. While there is currently little evidence to support this hypothesis, a broader analysis of international laboratory biosafety in the context of global health security is long overdue. How can the global community ensure that laboratories act safely when working with dangerous infectious diseases like COVID-19?
Such laboratories are necessary to understand and address infectious diseases. However, the reality is that these laboratories pose a biosafety risk, whether they’re in China, the United States, or anywhere else. Laboratory-acquired infections happen — one review identified more than 1,000 of them over a 25-year period, or approaching one infection per week on average. The most commonly identified causes are mishandled needlesticks or sharps, animal handling, spills or splashes, and accidental ingestion, but these account for only a portion of all laboratory-acquired infections. Inadvertent aerosols are suspected to cause a considerable proportion of the remaining infections, but in many cases the actual source of infection is never identified. In cases of contagious disease, where infected laboratory workers can then transmit the infecting agent to persons outside the laboratory, community outbreaks or even global pandemics can occur.
While we can mathematically quantify the corresponding risk to laboratory workers, extending that risk assessment to the local and global community poses numerous challenges. First, we need a full account of laboratories by location. Second, we need to know what specific activities each laboratory is performing, and with what specific biological agents. Third, we need to know what corresponding safety measures are in place and how reliable they are. And fourth, we need to know details of the surrounding community, including population demographics, density, mobility, and so on. None of this information is routinely collected at the international level; moreover, there is no international body, process, or standard to collect it.
To address this critical gap, the United States should work with the World Health Organization to establish an international safety regime for laboratories. Despite recent critiques of the organization’s handling of COVID-19 by the Trump administration, including its April announcement that the United States would halt funding to it and a May declaration at the 73rd World Health Assembly that it had “failed at its core mission,” it remains a linchpin in such efforts. The World Health Organization has successfully implemented similar international standards for infectious disease reporting and corresponding capacities, is a recognized authority on laboratory biosafety, and maintains the close working relationships with all governments needed to establish global scientific governance.
Step 1: Laboratory Registration
There is no comprehensive accounting of laboratories that work with dangerous biological agents, in the United States or on a global scale. In general terms, such laboratories fall into two non-mutually exclusive categories: diagnostic laboratories and research laboratories. Diagnostic laboratories receive clinical (i.e. human healthcare-related), animal, or environmental samples and perform tests to determine what biological agents or indicators of infection may be present. Research laboratories work with biological agents directly to improve our understanding of them and/or to develop and test medical countermeasures (e.g. diagnostics, therapeutics, vaccines) to address them.
Both diagnostic and research laboratories operate at increasing levels of biosafety depending on the agent and the type of work being performed. Biosafety level 1 is the lowest level of safety and is only utilized for agents that do not routinely affect humans. All diagnostic and research laboratories that handle potentially infectious clinical specimens, animal or environmental samples, or biological agents directly must do so at biosafety level 2 or above. Biosafety level 2 introduces practices, safety equipment, and facility features for safe handling of specimens, samples, and biological agents that are capable of causing moderate human disease, but do not commonly cause infection by aerosol. Biosafety level 3 builds on biosafety level 2 measures to address agents known to cause serious (potentially lethal) infection by aerosol. Lastly, biosafety level 4 extends biosafety level 3 measures to address agents posing the highest individual risk of life-threatening infection by aerosol and for which there is no vaccine or treatment. The World Health Organization provides international guidelines for safely working at each biosafety level in its Laboratory Biosafety Manual, with the purpose of reducing risk not just to the laboratory worker, but to the surrounding community and environment; the United States follows similar guidelines set forth in the Centers for Disease Control and Prevention’s Biosafety in Microbiological and Biomedical Laboratories. Consensus standards, such as the European Committee for Standardization’s Workshop Agreement 15793 “Laboratory Biorisk Management Standards,” have been developed to further harmonize biosafety requirements, both regionally and internationally.
The United States does maintain a record of laboratories that specifically work with biological select agents and toxins under the Federal Select Agent Program, which controls the possession, use, and transfer of dangerous biological agents (and toxins) deemed by the U.S. government as holding the potential to pose a severe threat to public, animal, or plant health. At the end of 2018, the program was overseeing a total of 253 registered “entities” working with biological select agents and toxins at various biosafety levels, most commonly level 3 (79% of entities). It’s a confusing nomenclature because “entities” is not synonymous with “laboratories”; in 2009, for example, the program reported more than 240 entities comprising at least 1,362 biosafety level 3 laboratories. A year later, that number grew to 1,495 level 3 laboratories, a number believed to reflect only a subset of the total number of level 3 laboratories in the United States (and across the globe), given the undetermined number of laboratories that do not work with biological select agents and toxins. Of note, the program reported 193 incidents in 2018 alone involving the accidental release of biological agents and toxins, the majority of which were the result of working without appropriate safety equipment; that’s an average of more than one accidental release every two days.
The World Health Organization’s International Health Regulations provide a potential vehicle for instituting such a legally binding laboratory registration mechanism at the international level. Under these regulations, the World Health Organization’s 196 states parties are required to share information on biological events within their respective territories that may pose a transboundary threat to other member states, including notification within 24 hours of events that may constitute a “public health emergency of international concern,” like COVID-19. The regulations could reasonably be expanded to include disclosure of qualifying laboratories and specifying biological agents being investigated and activities carried out by biosafety level. Qualifying laboratories would be expected to include any laboratory that poses a public health risk to the surrounding or global community. This would include any biosafety level 2 laboratory that works with contagious biological agents of moderate to severe lethality or for which there are no treatments or vaccines; all biosafety level 3 laboratories; and all biosafety level 4 laboratories. To ensure an appropriate balance of security and transparency, the corresponding database would be maintained on a restricted access website from which the World Health Organization could provide regularly updated public information, such as listing the total number of laboratories by biosafety level and providing information on broad international trends. (An existing example of this is the International Atomic Energy Agency’s Incident and Trafficking Database.) Because this information is already collected for other purposes, such a mandate should neither increase administrative burden on laboratories nor hinder peaceful research in any way.
Step 2: Laboratory Biosafety Accreditation
Next, registered laboratories must be rigorously assessed for safety assurance under an internationally accepted laboratory biosafety accreditation process. Laboratory infections and releases continue to occur in the face of widely acknowledged international guidelines set forth in the World Health Organization’s Laboratory Biosafety Manual, which identifies recommended laboratory practices, safety equipment, and facility features based on the biological agent being handled and the activity being performed. There is no internationally accepted accreditation process under the World Health Organization, or any other regime, for officially determining whether a particular laboratory and its people are “safe” to work with a particular biological agent in a particular way. However, the International Organization for Standardization’s “General Requirements for the Competence of Testing and Calibration Laboratories” — which comprehensively evaluates participating laboratories for compliance spanning personnel qualifications, written procedure validation, equipment calibration and maintenance, facility conditions, test quality, and records maintenance — provides a useful model for a similar global biosafety standard.
It is critical to understand that the laboratory itself is only one aspect of biosafety; even the best designed, constructed, and outfitted laboratory in the world depends on its people to possess the necessary skills to consistently apply best practices that minimize risk. Acquiring these skills, however, is not straightforward. There is no advanced biosafety degree program, and while training opportunities are available, they are neither standardized nor mandated at the international level. As such, it is generally acknowledged that most learning occurs in the course of performing laboratory work under supervision, similar to how a surgical resident learns to perform an operation by assisting a more senior surgeon and incrementally assuming responsibility over time. Thus, following the International Standards Organization example, any formal biosafety accreditation process must include a qualification component that certifies personnel for higher risk activities involving biological agents based on demonstrated proficiency, similar to certification by the World Institute for Nuclear Security Academy in the nuclear domain.
A formal laboratory biosafety accreditation process could be included in the updated International Health Regulations in conjunction with the above-described laboratory registration requirement, making it legally binding for all states parties. Compliance could reasonably be demonstrated and maintained via confidence-building measures leveraging a range of verification tools and/or bodies, from minimally invasive peer reviews by non-governmental organizations, to missions akin to those of the International Atomic Energy Agency’s International Physical Protection Advisory Service in the nuclear sector. Compliance audits might include laboratory inspections; review of records spanning over training, standard operating procedures, and equipment/facility maintenance and certification; and standardized proficiency testing with incremental corrective action planning.
Step 3: International Scientific Review Board — Establishment and Oversight
On balance, laboratories serve the public interest but do pose a risk, however small, that extends to the local and global community. Thus, in the same way that nuclear power plants are subject to peer-based oversight in order to safeguard surrounding communities and countries, some level of self-monitoring is necessary to ensure appropriate laboratory risk management on behalf of at-risk populations. The goal is to ensure uniform accountability of laboratories for the safety of their surrounding communities and environments, while preserving the ability to advance the understanding and management of infectious diseases. Currently, there is no formal international body for risk-based review and oversight of infectious disease-related research.
The World Association of Nuclear Operators provides a model for such an oversight body. This association conducts peer review, performance analysis, and training to ensure that the world’s nuclear power plants consistently meet international safety standards. Having a similar international scientific review board of qualified experts would provide the necessary assurance to local and global communities regarding the risks associated with specific types of high-risk infectious disease-related research. These risks would not only be considered, but mitigated to an international standard of risk acceptance. The board would be responsible for defining what types of research would apply, but general categories would be expected to include gain-of-function research to enhance transmissibility, infectiousness, or virulence of a qualifying biological agent; recombination research involving a qualifying biological agent or its sequence; de novo synthesis of wholly novel biological agents, or agents for which there is no universally available treatment or vaccine.
In practice, the board would be expected to operate under the following three-step process.
First, laboratories would submit a description of qualifying high-risk research identifying the project title and abstract; primary and collaborating institutions; researchers and their roles; scientific need, including critical knowledge gap(s) addressed; risk-benefit analysis; applicable safety provisions; and a technology development roadmap for corresponding countermeasure development so that the research has a tangible payoff to the public beyond the value of the knowledge itself. For example, in 2015, American and Chinese scientists, including scientists at the Wuhan Institute of Virology, demonstrated that a dangerous virus similar to Severe Acute Respiratory Syndrome could become readily transmissible from person to person with only minor genetic change. However, the research was not accompanied by corresponding medical countermeasure development, such as diagnostics, therapeutics, and/or vaccine platforms, which might have proved beneficial during the current COVID-19 pandemic.
Upon receipt of this description, peer review would determine whether the work is justified based on the scientific need, risk-benefit analysis, and technology development roadmap. This review would follow the model of scientific publication peer review, whereby articles are accepted for publication, returned for correction, or rejected.
Upon approval, work would commence under the board’s oversight, which would conduct initial, planned, and unplanned safety inspections, review progress and results, and provide a platform for peer-to-peer assistance, support, and training.
Step 4: International Policy Review Board – Establishment and Oversight
Finally, a forum for international dialogue is necessary to agree on standards aimed at reducing and/or repurposing the global laboratory footprint based on scientific and public health need and cumulative risk.
Scientific and Public Health Need
Any approach to reducing the number and/or purpose of existing or future laboratories must begin with an assessment of need. The need for diagnostic laboratories is based on “throughput,” i.e. the number of samples generated in a given area, similar to the way that the need for an elementary school is determined by the number of children residing in a certain sending district. By projecting the number of samples to be analyzed by test type, laboratory space can be allocated, sized, and outfitted accordingly. These diagnostic laboratories should meet biosafety level 2 standards, but are not required to meet higher level biosafety standards as long as proper protocols are followed.
The need for research laboratories is more challenging to calculate. Typically, research need is based in part on regional infectious disease burden, and in part on specific qualifications of a given laboratory. A more comprehensive approach may be to establish regional research agendas and scale laboratory footprints accordingly; these research agendas would also serve to enhance laboratory sustainability by informing and enabling international research collaboration, information-sharing, oversight, and supply chain management.
Cumulative Risk
Because no individual laboratory’s risk is zero, cumulative risk must be considered whenever laboratories are planned or programmed. While biosafety level 4 laboratories by definition house the highest risk category of work, with the highest risk biological agents, their limited number and rigorous biosafety standards may present a comparatively lower risk than biosafety level 2 and level 3 laboratories on aggregate. Each level 2 and level 3 laboratory comes not only with risks related to working with biological agents directly, but also chemical, electrical, and force majeure (fire, earthquake, etc.) risks. More importantly, dangerous biological agents, as well as unknown samples, are commonly handled at lower biosafety levels.
For example, while much has been made of the Wuhan Institute of Virology’s biosafety level 4 laboratory (which opened in 2017), any research with related coronaviruses would most likely have been conducted in its longstanding level 2 or level 3 laboratories. Bat samples being evaluated for the presence of coronaviruses would most likely be unpacked and prepared in a biosafety level 2 laboratory, inside a biosafety cabinet, and then transferred to a biosafety level 3 laboratory for further research as appropriate. Even the comparatively lethal coronavirus responsible for the 2003 outbreak is handled at no higher than the biosafety level 3, and only if the virus is being knowingly cultured or characterized.
Summary Recommendations
Because certain laboratories pose a risk to local and global communities, as well as animal populations and the environment, steps must be taken to ensure their safety, and to ensure accountability at the international level. The necessary steps include laboratory registration; biosafety accreditation; self-disclosure of qualifying high-risk research; peer review and oversight of disclosed high-risk research by an international scientific review board of qualified experts; and an international dialogue to establish standards for scaling the global laboratory footprint based on scientific and public health need weighed against cumulative risk. Together, these steps will reduce the risk of far-reaching laboratory accidents and mishaps while enabling the global scientific community to continue to battle pandemic threats unabated.
Dr. Richard Pilch, a physician by training, is the Director of the Chemical and Biological Weapons Nonproliferation Program at the James Martin Center for Nonproliferation Studies. He has led multiple threat reduction programs on behalf of the U.S government, assessing and addressing biological warfare, bioterrorism, and public health emergencies of international concern.
Miles Pomper is a Senior Fellow at the James Martin Center for Nonproliferation Studies, a part of the Monterey Institute of International Studies, and Chair of the Fissile Materials Working Group, the leading international nongovernmental coalition on nuclear security.
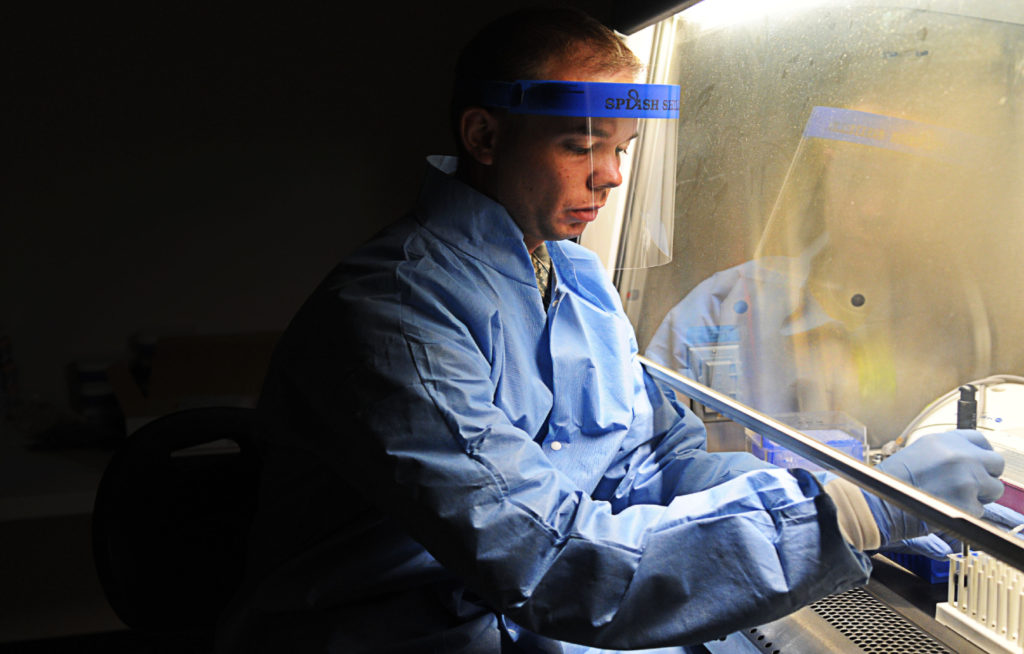
Image: U.S. Air Force (Photo by Senior Airman Lauren Main)

