COVID-19 and the U.S. Military

As the United States endures its third COVID-19 wave, how has the military responded to the challenge? While the armed forces are inextricably a part of American society, has it performed better or worse relative to the civilian population?
The Center for Strategic and International Studies has tracked the pandemic’s effect on the military since mid-March and has been publishing weekly updates on the number of infections, deaths, military responses, and operational impact. Raw data come from the Department of Defense, supplemented by the Center for Disease Control and the Johns Hopkins Coronavirus Resource Center. What follows is an assessment of what the data have shown.
Despite significant early disruptions, the U.S. military has been able to maintain training, deployments, and even recruitment during the novel coronavirus pandemic. Infection rates among servicemembers are slightly lower than the country at large, and fatality rates are much lower. Military bases are not infection hot spots. In short: Precautions that the military took, after some initial missteps, have been effective. However, the novel coronavirus pandemic’s long-term effect on the military is uncertain. It might be a passing wave that disappears after two years, or it might make fundamental changes in the armed forces’ structure.
The Military Experience: Two Waves and an Emerging Third
The U.S. military, like the rest of the United States, has so far experienced two major waves of new infections and the beginnings of a third. The first wave peaked in mid-April at roughly 250 new Department of Defense cases a day before declining in May. The second much larger wave peaked in mid-July at around 800 new cases a day. New cases steadily declined from the second wave peak and bottomed out in mid-September. They have recently begun to rise again, constituting a third wave. The chart below on new military cases of COVID-19 shows these waves.
Figure 1: New Defense Department COVID-19 Cases
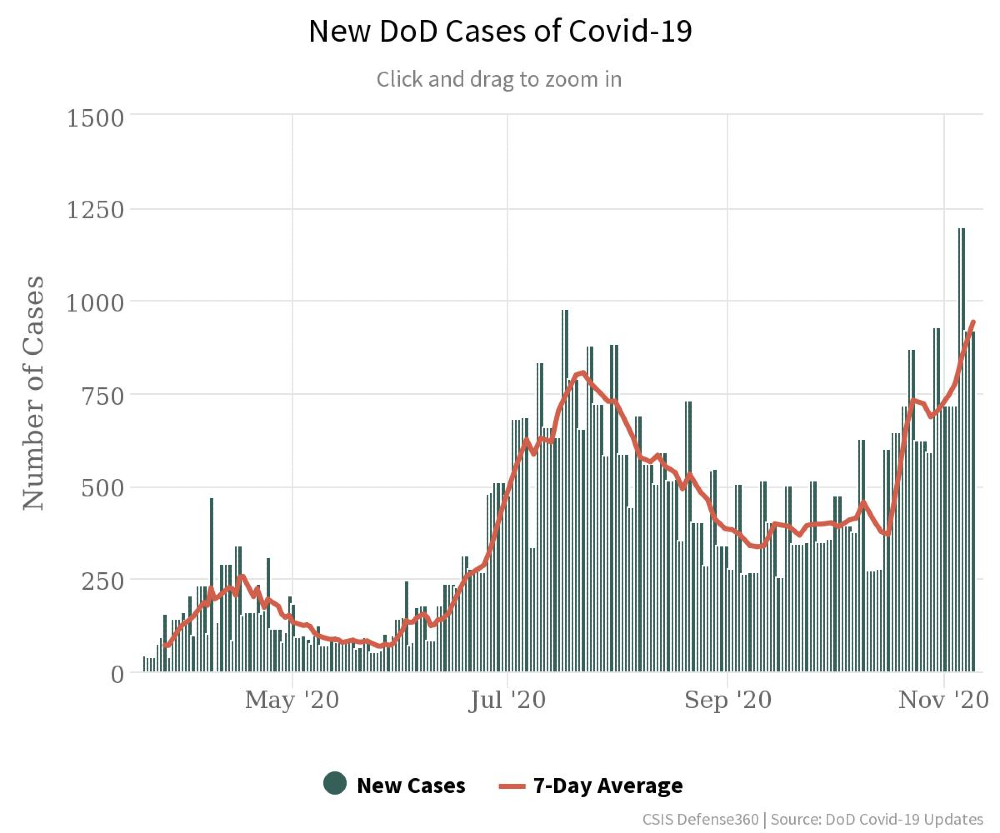 Source: Chart generated by the authors. See the full interactive at CSIS Defense360.
Source: Chart generated by the authors. See the full interactive at CSIS Defense360.
As of Nov. 6, the Defense Department had a cumulative total of 89,000 cases. Most cases (roughly 60,000) have been military servicemembers (active-duty and reserve), averaging 67 percent of all Department of Defense cases over the course of the pandemic. Defense Department civilians constitute the next major group of positive cases, at 14,000 cases, and have averaged 16 percent of total cases. The two smallest groups, dependents and contractors, average 10 and 7 percent of total cases in the military, with about 9,000 and 6,000 cases respectively.
The data on infections and fatalities are good, though not perfect. Data come from reports submitted by the military services and defense agencies to the Joint Staff crisis management team. Defense Department guidance requires that all individuals report if they become infected. As a practical matter, it would be nearly impossible for a full-time employee ― whether a military, civilian, or contractor ― to be sick with the novel coronavirus and absent from work without the organization knowing about it. Asymptomatic individuals are more difficult to identify in the Department of Defense, as in the country as a whole. The military’s formal testing program picks up some asymptomatic cases, though not all, as does civilian testing through an individual’s health care program. Data for reservists are likely less complete since they are not present every day though they also are required to report.
Figure 2: Cumulative Cases Across the Defense Department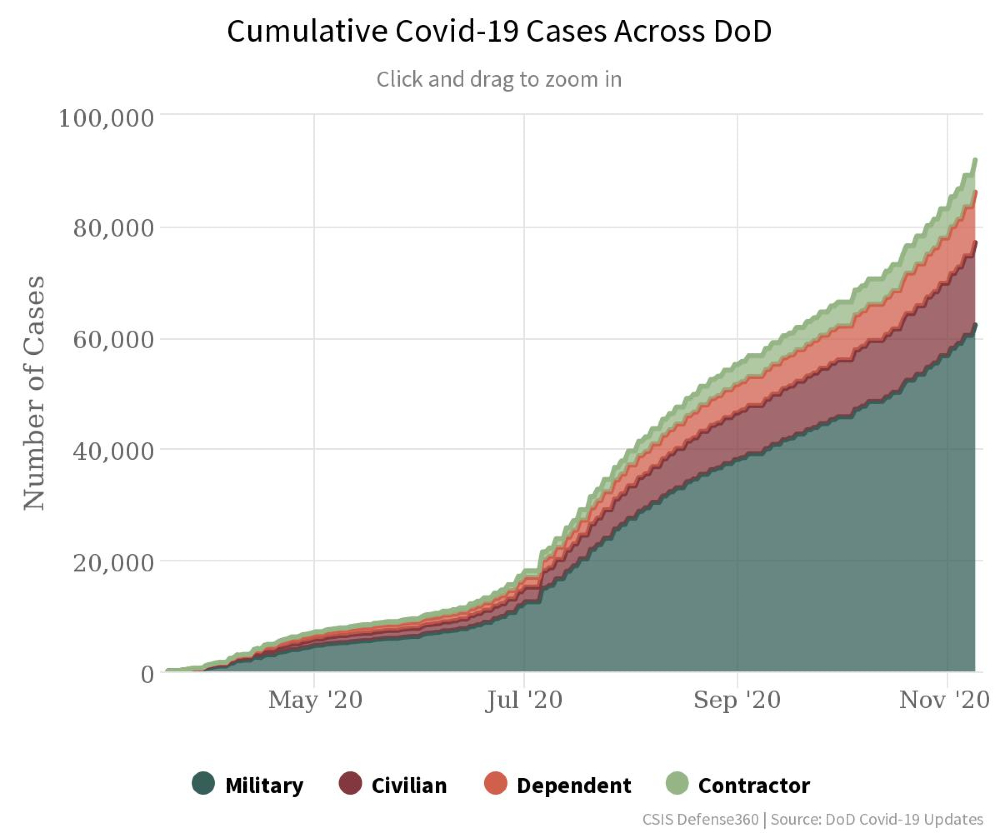
Source: Chart generated by the authors. See the full interactive at CSIS Defense360.
Effect on Operations and Readiness
In response to rising COVID-19 cases, the Defense Department issued an order on March 25 prohibiting the deployment of servicemembers for 60 days to prevent the spread of the novel coronavirus. It subsequently issued revised guidelines mandating that they be tested for COVID-19 and undergo a 14-day quarantine prior to deployment. Further, the Defense Department canceled, postponed, or significantly reduced major military exercises, such as Defender Europe 2020.
The Defense Department established a four-tier testing program for the entire force, prioritizing strategic and fielded forces, followed by forward deployed troops and then the rest of the force. This will likely be the priority for vaccination when a vaccine becomes available.
As the rate of new COVID-19 cases slowed, the military resumed high-level training exercises with caution. The large Baltic Operations and Rim of the Pacific naval exercises were held entirely at sea due to COVID-19 concerns. Navy ships have also been kept out at sea longer and are making fewer port calls to minimize the risk of infection. Soldiers participating in exercise Saber Junction were required to wear masks and carry hand sanitizer. These precautions appear to have been effective in preventing the spread of COVID-19. For instance, thousands of U.S. personnel completed exercise Saber Junction without a single positive case of the novel coronavirus.
Additionally, COVID-19 concerns led all the military services to pause basic training for new recruits and implement new safety procedures. Despite their initial reluctance, Army officials stopped sending recruits to basic training after one recruit tested positive for the novel coronavirus. After this two-week pause, new recruits were continuously tested for COVID-19 and monitored with daily health assessments during basic training, precautions that reduced the spread of the novel coronavirus. The Air Force also paused basic training after at least four recruits contracted the virus, while the Marine Corps stopped sending recruits to boot camp on Parris Island after hundreds tested positive for COVID-19. Air Force basic training reopened with smaller class sizes and a 14-day quarantine for new arrivals, as did the Marine Corps’ boot camp. Navy basic training followed a similar path.
Performance Is Generally Consistent Across Services
COVID-19 infection rates (number of cases divided by the total service personnel) are about the same in the Army, Navy, and Marine Corps: 0.033 for each (as of Nov. 6). The Air Force rate is lower, 0.022, likely because its activities don’t involve large groups getting together. The National Guard, which is tabulated separately, has the lowest infection rate, 0.016, but that may be an artifact of lower reporting of part-time personnel.
This consistent performance across services has not always been the case. At the beginning of the pandemic, the Navy had the largest number of cases, with over a thousand cases more than the next largest service (Army) by the end of May (from 2,400 to 1,400). The difference in infection rates was even more striking, the Navy’s being three times as high (the Navy 0.6 percent, the Army 0.2 percent). This disparity makes sense in the context of high-profile outbreaks among Navy ships, the most notable being the USS Roosevelt, which had more than 1,200 cases. The Navy responded with aggressive testing and may have picked up more positives.
However, the proportion began to shift as the summer progressed, with Army cases eventually overtaking the number of Navy cases on June 26. Army cases now make up by far the majority of cases among the services, with 18,000 out of 49,000 total military cases, 8,000 more cases than the Navy, which now has the second largest number of cases. The Army (including the Army Reserve) have by far the largest number of personnel of the services, so while the rate is the same, the total numbers are naturally higher.
The rise in Army cases may reflect the Army’s resumption of most training and exercises in early summer. It may also reflect the Navy reverting to the mean, as it improved its pandemic practices to prevent further outbreaks on ships and thus reduced its infection rate.
The Military Is Not Driving the Level of Cases Nationally
Historically, armies have been breeding grounds for disease. Indeed, the 1918 influenza pandemic likely began in the military and spread as a result of training exercises, crowded accommodations, and transfers around the country and overseas. For most of history, disease has caused more casualties than battles. Thus, many observers were ready to believe that the U.S. military was a disease hot spot, and several articles had that implication.
That turns out not to be true. As of Oct. 22, the disease incidence for the military was 2,387 cases per 100,000 (52,321 cases in a population of 2,191,000, active and reserve). This is slightly lower than for the overall U.S. population, which is 2,527 cases per 100,000 (8,338,000 cases in a population of 330 million). The total Department of Defense population has an even lower incidence, 1,587 cases per 1,000,000 (76,484 cases in a population of 4,818,000). (The total Department of Defense population consists of 2,191,000 members of the military, 1,596,200 dependents, 775,000 government civilians, and 384,000 contractors.)
This disparity is not caused by a lower rate of military testing. The Department of Defense tests 40,000 servicemembers per week or 0.39 percent per day. The United States, as a whole, tests about 1.1 million citizens per day or 0.33 percent. (Whether either level of testing is adequate is another issue.)
The reasons for this lower incidence are likely twofold. The military has more powerful levers for social control than the civilian community. Even though servicemembers tend to be young and might be willing to take more risk, social controls reduce their risky behaviors. Other members of the defense community, though not under the tight control of the Uniform Code of Military Justice, are required to conform to Defense Department, state, and local guidance. The second reason is the widespread imposition of precautions: personal protective equipment, social distancing, quarantine, and telework.
Because these infection rates are averages, there will inevitably be variations from base to base. Some military bases will have higher rates of infection than the community around it. However, most bases will have lower infection rates. That’s good news for bases and their surrounding communities because it reduces the tension that hosting a military base inevitably causes.
The military has contained infections on overseas bases, even when the rates are higher than in the host nation. This has been a particular concern in Asia, where countries like Australia, South Korea, and Japan, which host large numbers of U.S. servicemembers, have had much more success in containing the pandemic than the United States and Europe. Concerns arose that the routine rotation of personnel from the United States would bring disease with them. However, despite some scares about hot spots, infections have been limited to the bases. Aggressive countermeasures, like quarantining, have been successful, with procedures instituted by U.S. forces in Korea constituting a model.
This containment has been critical in maintaining U.S. presence overseas and preventing the opening of a vulnerability. Had U.S. forces interrupted the usual unit and personnel rotations, the sudden power vacuum might have induced regional instability and conflict. At the very least, it would have inflicted reputational damage on the U.S. military.
The Military Is Not Immune From the Rest of Society
Although the Defense Department has a lower infection rate than society overall, the profile of military cases has nevertheless closely tracked the profile of cases in the U.S. population. This is clearly illustrated by overlaying the graph of new Defense Department cases of COVID-19 onto that of new cases in the U.S. population. The two major waves of COVID-19 cases, and possibly a third, have emerged and declined among military personnel at roughly the same rates as those reported among the broader U.S. population. This suggests that the military is affected like the U.S. population and cannot fully isolate itself. As the nation goes, so does the military.
Figure 3: Comparing National and Department of Defense Case Trends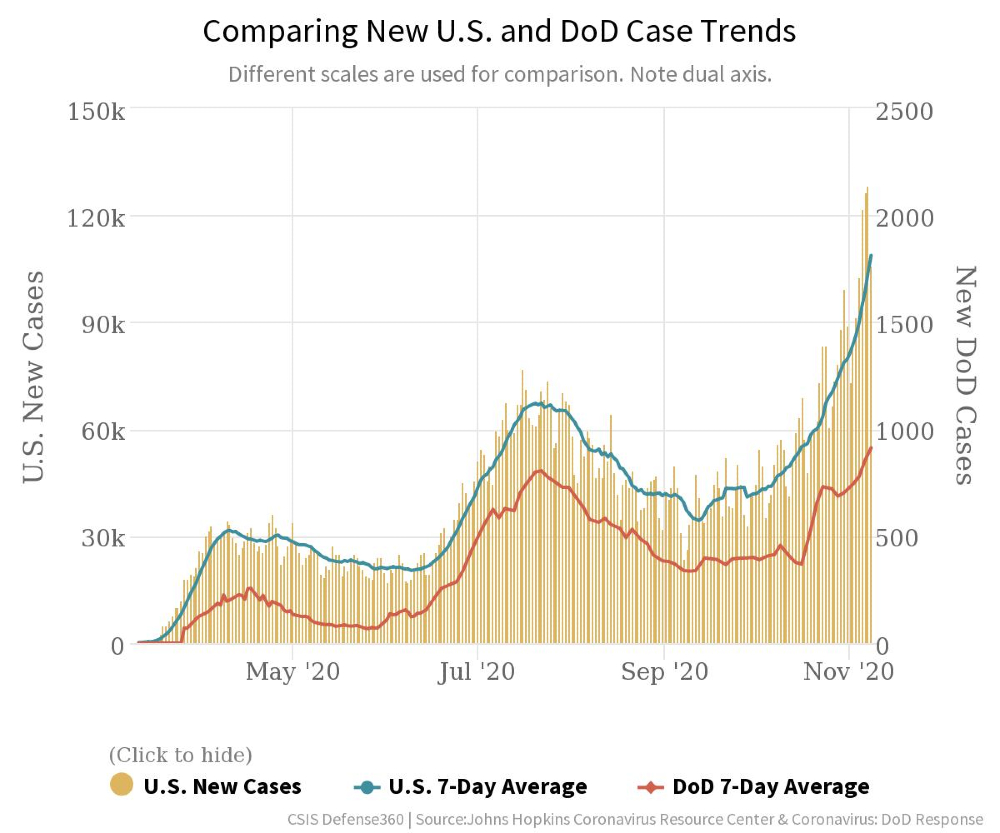
Source: Chart generated by the authors. See the full interactive at CSIS Defense360.
The Military’s Low Fatality Rate
According to Defense Department data released Oct. 22, the military’s fatality rate is 0.015 percent (eight deaths for 52,321 cases): One servicemember dies for every 6,500 servicemembers who are infected. For the United States as a whole, it is 2.7 percent (222,663 deaths for 8,378,377 identified cases), 180 times as much. That the military has a lower fatality rate is not surprising. Its population is young and healthy, with good health care. The military has none of the elderly who are so susceptible to the infection. What is surprising is how much lower the fatality rate is.
The military inadvertently did an experiment that illustrates this disparity. When the USS Roosevelt tied up at Guam last March and April after the infection spread through the ship, the entire crew was isolated, tested, and monitored. Of the 1,200 crew members infected, 45 were hospitalized for observations and seven went to intensive care, but only one died.
What is also surprising is that the broader Defense Department community (military, dependents, and government civilians) has a low fatality rate: 0.13 percent (102 deaths for 76,484 cases) or about one-twentieth of the overall U.S. population. Although government employees are not on average as young as military personnel and dependents are not as fit, civilians are healthy enough to be working, and dependents are young enough to be family members of a servicemember. Both groups have good health care.
The good news for the armed forces is that continuing a high level of training and operations, protected by the evolved procedures, does not impose undue risks. If an emergency were to occur, and more forces had to deploy, the risks would rise but not be crippling or catastrophic. This contrasts with the military’s experience during the 1918 influenza pandemic when young people were particularly susceptible, and the military had tens of thousands of fatalities.
Long-Term Structural Effects Are Uncertain
Although the novel coronavirus pandemic dominates our lives today and restructures the activities of every organization, that will not continue forever. What happens to national security organizations when the novel coronavirus pandemic finally fades away?
Some things are nearly certain to happen. The Defense Department’s medical stocks will be replenished and, likely, expanded to prepare for a future emergency. The military’s medical research organizations will get a budget lift regardless of what happens to the rest of the department, as the nation will want to strengthen its medical response.
The proposed restructuring of the Defense Department medical community ― which, if enacted, would make it smaller and focused on combat operations rather than on the care of dependents and retirees ― will likely be put on hold. Even though this restructuring has little to do with the pandemic, retiree groups have strongly opposed any changes to military medicine, and Congress will likely be wary of any diminution in medical capability.
Beyond that, it may be that in two years, when life may return to some semblance of normal, the Defense Department returns to its pre-pandemic focus on military training, deployments, and reorienting itself for great-power competition, particularly in the Western Pacific.
On the other hand, Congress might direct the Defense Department to build pandemic-specific kinds of capabilities to help protect the military itself and the civilian population during the next public health crisis. These might include building more hospital ships or creating more specialty units. Fighting disease and countering domestic emergencies might be added as core Defense Department missions. The military might be asked to get more involved in the national pandemic response.
This may be a lot to ask as the Defense Department tries to reorient itself for great-power conflicts, even as the massive increase in federal debt and a focus on domestic affairs might squeeze the defense budget. Further, the crisis is not over. Experts expect the national death toll to approach half a million by February and, as the data show, the military is not completely separate from the rest of society. At some point, this increase will threaten the military’s ability to train and deploy. That may create a power vacuum overseas just as a new administration is taking office.
Col. Mark Cancian, U.S. Marine Corps (ret.), is a senior adviser with the Center for Strategic and International Studies International Security Program, where he writes about military forces, budgets, and operations. Cancian spent over three decades in the U.S. Marine Corps, active and reserve, serving as an infantry, artillery, and civil affairs officer and on overseas tours in Vietnam, Desert Storm, and Iraq (twice). He holds a bachelor’s degree and an MBA from Harvard University.
Adam Saxton is a research associate with the International Security Program at the Center for Strategic and International Studies, where he supports research related to U.S. force structure, great-power conflict, and the international order.
Nidal Morrison is a research intern with the International Security Program at the Center for Strategic and International Studies.
Image: U.S. Air National Guard (Photo by Senior Airman Kregg York)

